By clicking “Accept All Cookies”, you agree to the storing of cookies on your device to enhance site navigation, analyze site usage, and assist in our marketing efforts. View our Privacy Policy for more information.
Average Weight Loss after Gastric Sleeve
Nutrition and Dietary Guidance The dietary journey post-gastric sleeve surgery typically involves progressive phases designed to support healing, adapt to the reduced stomach size, and facilitate sustainable weight loss.
By
March 13, 2024
Embarking on the path of weight loss through any weight loss surgery is a transformative journey, offering hope and health improvements for those struggling with excess body weight. This procedure, also known as sleeve gastrectomy, involves the removal of a portion of the stomach, creating a sleeve-like pouch and aiding in weight loss. In this comprehensive guide, we'll explore the average weight loss expectations, the timeline, and the transformative impact on overall health.
Understanding Gastric Sleeve Surgery:
Gastric sleeve surgery, a form of bariatric surgery, is a significant step towards achieving weight loss goals. This laparoscopic procedure involves reducing the stomach size, affecting hormones that regulate appetite and contributing to effective weight management. Other weight loss surgeries like gastric bypass and laparoscopic adjustable gastric band serve different purposes, but gastric sleeve surgery stands out for its efficiency and effectiveness.
The Early Stages: Immediate Post-Surgery:
The initial phase following gastric sleeve surgery is marked by rapid weight loss. Patients experience substantial changes in the first few weeks, with an initial surge in weight loss due to lower calorie intake and the body adapting to the new stomach shape.
Nutrition and Dietary Guidance
The dietary journey post-gastric sleeve surgery typically involves progressive phases designed to support healing, adapt to the reduced stomach size, and facilitate sustainable weight loss. The initial phase, often in the immediate post-operative period, emphasizes clear liquids and gradually transitions to pureed and soft foods. This phase allows the stomach to heal while providing essential hydration and nutrients. As patients progress, they advance to more textured and solid foods, ultimately embracing a balanced and nutrient-dense diet. The focus shifts towards incorporating lean proteins, vegetables, fruits, and whole grains while avoiding sugary and high-calorie foods. Ongoing collaboration with healthcare professionals, including dietitians, ensures a personalized approach that aligns with individual needs and promotes a successful and healthy post-surgery dietary journey.
As the stomach size is reduced, and in some cases, parts of the digestive tract are rerouted, the ability to absorb certain vitamins and minerals may be compromised. This makes postoperative supplementation crucial to prevent nutritional deficiencies and support overall well-being.
- Vitamin B12: One of the essential vitamins often affected is B12, vital for nerve function and the production of red blood cells. Due to changes in stomach anatomy, patients may struggle to absorb B12 from food alone. Regular B12 supplementation or injections become imperative to prevent deficiencies.
- Iron: Iron deficiency is common after bariatric surgery, leading to symptoms like fatigue and weakness. Iron supplementation is frequently recommended to ensure an adequate supply for essential functions like oxygen transport in the blood.
- Calcium and Vitamin D: The relationship between calcium and vitamin D is crucial for bone health. With alterations in the digestive system, calcium absorption may be impaired. Supplementation, along with sufficient vitamin D, helps maintain bone density and prevent fractures.
- Multivitamins: A well-rounded multivitamin is often prescribed to cover a spectrum of essential nutrients. This may include vitamins A, C, E, and K, as well as various B vitamins, to address potential gaps in the diet.
- Regular Monitoring: Post-bariatric surgery patients should undergo regular blood tests to monitor nutrient levels. This enables healthcare professionals to tailor supplementation plans to individual needs, preventing deficiencies and promoting optimal health.
- Patient Education: Empowering patients with knowledge about the importance of adhering to their prescribed supplement regimen is crucial. Understanding the role of each vitamin and mineral and the potential consequences of deficiencies motivates individuals to prioritize their postoperative nutritional needs.
Monthly Weight Loss Timeline:
Understanding the monthly weight loss timeline is essential for patients seeking gastric sleeve weight loss results. On average, individuals can expect to lose between 5 to 15 pounds per week in the initial two to three months. This remarkable weight loss pace contributes significantly to achieving excess weight loss goals.
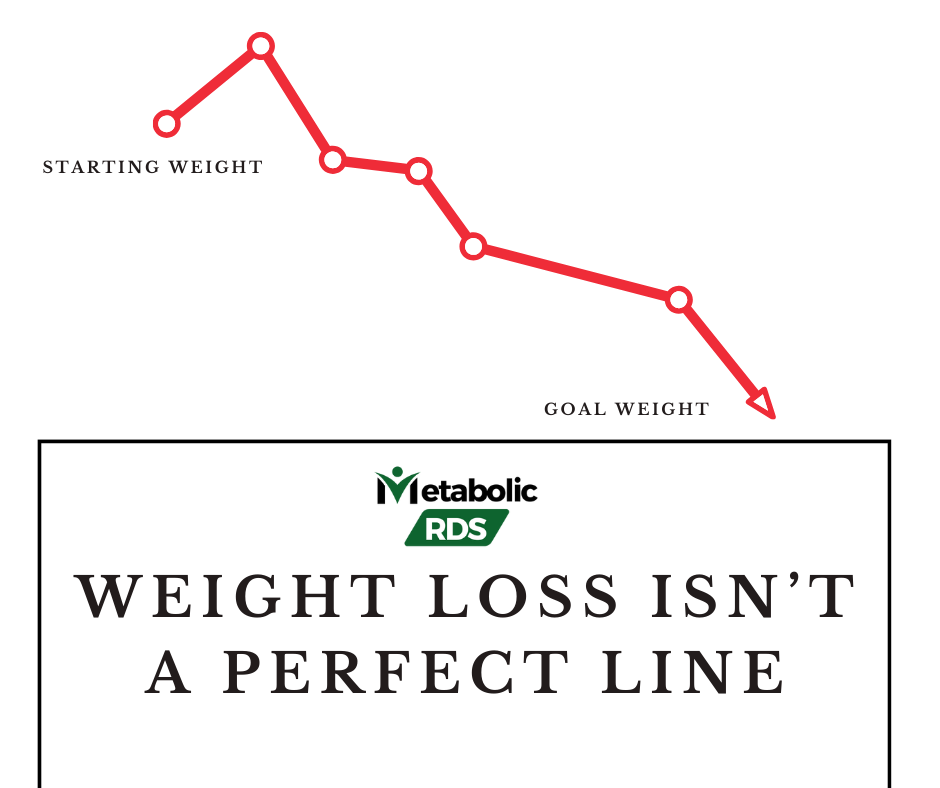
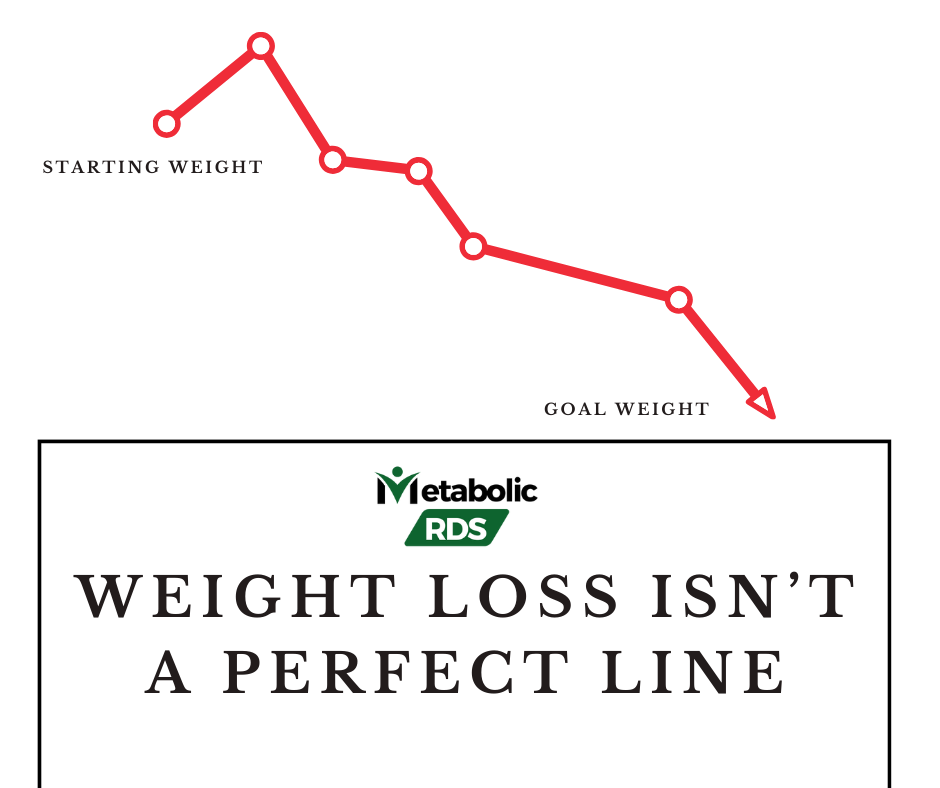
Weight loss, often measured on scales, reflects the overall reduction in body mass, which can include fat, muscle, and water. However, a comprehensive understanding of body composition involves assessing the distribution of fat and muscle, offering a more nuanced perspective. Additionally, weight can fluctuate throughout the day due to factors like hydration, food intake, and bowel movements.
Focusing on long-term trends rather than daily fluctuations is key.
Total Weight Loss Expectations:
Within the first year, patients can achieve approximately 60-70% of their excess body weight loss. While these figures provide a general guideline, individual outcomes vary based on factors such as starting weight, adherence to guidelines, and overall health. A weight loss calculator can assist in setting realistic goals, ensuring a steady and sustainable journey.
Check Out This Weight Loss Calculator For Bariatric Surgery!

Body Mass Index and Bariatric Procedures:
Body Mass Index (BMI) plays a crucial role in determining eligibility for bariatric procedures. Gastric sleeve surgery is often recommended for individuals with a BMI of 40 or higher or those with a BMI of 35 or higher who have obesity-related health conditions. Understanding BMI and its implications helps individuals and healthcare professionals make informed decisions regarding the most suitable weight loss procedure.
It's important to note that an "ideal" body weight is subjective and varies among individuals. Factors such as muscle mass, body composition, and distribution of fat play a role in determining a healthy weight. Consulting with healthcare professionals, including dietitians and surgeons, helps establish realistic and personalized goals.
A Quick Note About BMI: Pros and Cons
Pros: BMI serves as a quick and easy screening tool to assess general body weight relative to height. It provides a standardized measure that can be useful for population health studies, allowing for broad comparisons across different groups. Additionally, it is a cost-effective and non-invasive method, requiring only height and weight measurements.
Cons: Critics argue that BMI has limitations, as it doesn't differentiate between muscle and fat, leading to potential misclassifications of individuals with higher muscle mass. It also doesn't account for variations in body fat distribution, overlooking the importance of visceral fat. Furthermore, BMI doesn't consider factors such as age, sex, or ethnicity, making it a somewhat generalized measure that may not reflect individual health accurately. As with any tool, understanding its limitations is crucial for a nuanced interpretation of results.
When you work with a Dietitian that has a lot of experience in weight loss and weight management, they can help you understand what a healthy weight means to you and not just the BMI or other guidelines; you're a person not a number in a box.
Comparing Gastric Sleeve to Other Weight Loss Approaches:
Different weight loss interventions yield varying outcomes. Gastric sleeve surgery, gastric bypass surgery, and medications like GLP-1 agonists present distinct benefits and considerations.
- Gastric Sleeve vs. Gastric Bypass:
Gastric bypass involves rerouting the digestive system, leading to both restriction and malabsorption. While weight loss is significant, it may also result in more nutritional considerations due to decreased absorption. Gastric sleeve, on the other hand, focuses on restriction alone, reducing stomach size without rerouting the digestive tract. The choice between the two depends on individual health needs, preferences, and potential risks.
- Gastric Sleeve vs. Weight Loss Medications (GLP-1 Agonists):
Medications like GLP-1 agonists work by regulating appetite and slowing digestion. They can be an option for individuals who may not qualify for or prefer non-surgical interventions. However, their effectiveness varies among individuals, and weight loss may be more gradual compared to surgical procedures. Combining medication with lifestyle changes may optimize outcomes.
You can read more about our thoughts on GLP-1 and weight loss medications here
Beyond the First Year: Long-Term Success:
As the initial year progresses, the pace of weight loss may slow, and some patients might experience plateaus. However, maintaining a balanced approach with a nutrient-dense diet, regular physical activity, and ongoing medical care enhances long-term success. Gastric sleeve surgery offers benefits beyond just weight loss, often improving conditions such as type 2 diabetes, high blood pressure, and sleep apnea.
Related Health Improvements:
Gastric sleeve surgery goes beyond addressing excess weight; it often leads to substantial improvements in related health conditions. Conditions like type 2 diabetes show marked enhancements, high blood pressure normalizes, and sleep apnea symptoms reduce, promoting better overall well-being.
Hernia Management:
One significant benefit of gastric sleeve surgery is its potential to address hernias. Excess weight and obesity can contribute to the development of hernias, particularly in the abdominal region. The reduction in stomach size during gastric sleeve surgery may alleviate pressure on the abdominal wall, reducing the risk of hernias and providing relief for those who may have pre-existing hernias.
Holistic Approach to Post-Surgery Care:
Achieving success post-surgery involves more than just the physical aspect. Embracing a holistic approach to health, including mindful eating habits, regular exercise, and mental well-being, contributes to long-term positive outcomes. Collaborating with healthcare professionals, including dietitians and support groups, ensures ongoing support for patients.
Navigating Challenges: Plateaus and Adjustments
While gastric sleeve surgery can yield remarkable results, some patients may face challenges, such as weight loss plateaus or the need for adjustments. Understanding that individual journeys differ and that occasional adjustments to the surgical procedure might be necessary ensures a more realistic and informed approach.
Mental and Emotional Wellness:
Exploring the mental and emotional aspects of post-surgery life is crucial for long-term success. Many individuals experience positive changes in self-esteem, body image, and mental well-being. Addressing any challenges, seeking support through counseling or support groups, and developing healthy coping mechanisms contribute to overall wellness.
Lifestyle Changes for Lasting Health:
Beyond the surgery itself, maintaining lifestyle changes is integral to lasting health improvements. Patients are encouraged to adopt sustainable habits, including regular physical activity, balanced nutrition, and stress management. These lifestyle changes not only support weight maintenance but also contribute to overall well-being.
Navigating the Social Aspect:
The social aspects of life post-surgery can present unique challenges. Patients may encounter questions, comments, or even misconceptions from friends, family, or colleagues. Establishing open communication, educating others about the surgery, and seeking support from those who understand contribute to a more positive social experience.
Celebrating Non-Scale Victories:
In addition to the scale, recognizing and celebrating non-scale victories is essential. Non-scale victories include improvements in energy levels, better mobility, and enhanced overall health. These achievements, both big and small, highlight the holistic transformation that comes with gastric sleeve surgery.
Life After Gastric Sleeve Surgery:
As patients navigate life after gastric sleeve surgery, the focus shifts to sustaining positive changes and embracing a newfound sense of well-being. The journey extends beyond the surgical procedure, encompassing a commitment to health, self-care, and a fulfilling life. The support of healthcare professionals, ongoing education, and a resilient mindset contribute to a successful post-surgery life.
Nutrition needs change from the early phases to the long-term phase of weight maintenance. We offer meal plans that focus on bariatric dietary needs. Book an appointment with us for a meal planning session!

Conclusion:
In conclusion, understanding the average weight loss after gastric sleeve surgery is a crucial aspect of the transformative journey towards a healthier and more fulfilling life. The procedure offers not only remarkable weight loss results but also significant improvements in overall health. As patients navigate the post-surgery path, every step forward becomes a testament to their commitment to lasting well-being.